CDC’s 2025 Flu Projections: Higher Virulence, Early Vaccination Urged

The Centers for Disease Control and Prevention (CDC) has released its 2025 flu season projections, indicating a concerning increase in strain virulence and strongly advising early vaccination for optimal public health protection.
The Centers for Disease Control and Prevention (CDC) has recently issued a critical health advisory regarding the upcoming 2025 flu season projections, signaling a potentially more aggressive influenza season. This advisory underscores the importance of proactive health measures, particularly early vaccination, to safeguard public health. Understanding these projections and acting upon expert recommendations is vital for individuals and communities across the United States.
understanding the 2025 flu season projections
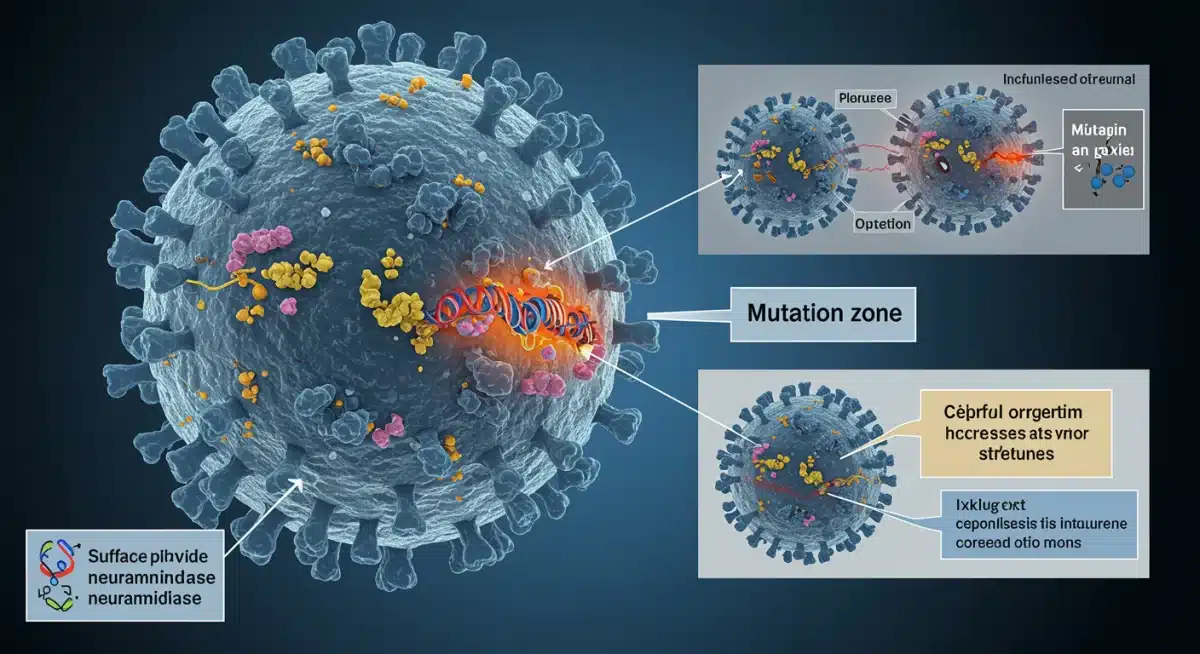
The CDC’s annual flu season projections are a cornerstone of public health preparedness, offering crucial insights into anticipated viral activity and strain characteristics. For 2025, these projections highlight a significant concern: an expected increase in strain virulence. This means the circulating influenza viruses are likely to cause more severe illness, potentially leading to higher rates of hospitalization and complications compared to previous years. These forecasts are not mere predictions but are based on extensive global surveillance data, genetic sequencing of circulating strains, and epidemiological patterns observed in the Southern Hemisphere, which often foreshadow the Northern Hemisphere’s flu season.
The agency monitors a complex interplay of factors to arrive at these conclusions. This includes tracking the emergence of novel variants, assessing the effectiveness of current vaccines against these strains, and analyzing population immunity levels. The goal is to provide a timely warning that allows healthcare systems, vaccine manufacturers, and the public to prepare adequately. The emphasis on early vaccination stems directly from this comprehensive data analysis, aiming to build robust community immunity before the flu season gains momentum.
the science behind virulence forecasts
- Genetic drift: Continuous, small changes in the flu viruses’ genes, leading to new strains.
- Antigenic shift: Abrupt, major changes in the flu A viruses, resulting in new subtypes.
- Global surveillance: Monitoring flu activity worldwide, especially in the Southern Hemisphere.
- Strain characterization: Laboratory analysis to identify dominant and emerging strains.
These scientific underpinnings ensure that the CDC’s advisories are grounded in robust evidence. The 2025 projections, therefore, represent a carefully considered assessment of evolving viral threats, urging a collective and informed response to protect public health. The public’s understanding of these projections is as important as the projections themselves, as it directly influences individual health decisions.
In conclusion, the 2025 flu season projections are a serious call to action, rooted in scientific observation and global health data. They underline the dynamic nature of influenza viruses and the continuous need for vigilance and adaptation in public health strategies. Preparing for a season with higher virulence means prioritizing preventative measures, with vaccination at the forefront.
why higher strain virulence is a concern
When the CDC warns of higher strain virulence, it signals a potential for more severe health outcomes across the population. Virulence refers to the degree of pathogenicity of a microorganism, or its ability to cause disease. A more virulent flu strain means that individuals who contract the virus are more likely to experience intense symptoms, require medical intervention, and face a higher risk of complications such as pneumonia, bronchitis, or even death. This increased severity can place immense pressure on healthcare systems, leading to overcrowded hospitals, shortages of medical staff, and strain on emergency services. Vulnerable populations, including the elderly, young children, and those with underlying health conditions, are particularly at risk, but even healthy individuals can experience significant illness.
The impact of higher virulence extends beyond individual health. It can disrupt daily life, affecting schools, workplaces, and the economy as a whole. Increased absenteeism due to illness or caregiving responsibilities can lead to significant productivity losses. Furthermore, the economic burden associated with heightened healthcare utilization and treatment costs can be substantial, both for individuals and the healthcare system. The CDC’s advisory is thus a multifaceted warning, addressing not only the direct health consequences but also the broader societal implications of a more aggressive flu season.
potential complications from virulent strains
- Pneumonia: A serious lung infection, often bacterial, that can follow influenza.
- Bronchitis: Inflammation of the bronchial tubes, leading to coughing and breathing difficulties.
- Exacerbation of chronic conditions: Worsening of existing heart disease, asthma, or diabetes.
- Secondary bacterial infections: Infections that can occur after the flu has weakened the immune system.
Recognizing these potential dangers underscores the urgency of preventive measures. The higher the virulence, the greater the imperative to build immunity through vaccination, reducing the chances of severe illness and mitigating the strain on public health resources. The goal is to minimize the spread and impact of these more potent strains. By understanding the implications of increased virulence, individuals can make informed decisions about their health and contribute to community resilience.
In summary, higher strain virulence is a significant concern because it translates to more severe illness, increased healthcare burden, and broader societal disruptions. This makes early vaccination an even more critical component of public health strategy.
the critical importance of early vaccination
The CDC’s recommendation for early vaccination against the 2025 flu season is not merely a suggestion; it is a critical public health directive designed to maximize protection. Vaccinating early allows the immune system sufficient time to build a robust antibody response before influenza viruses begin to circulate widely. Typically, it takes about two weeks after vaccination for antibodies to develop and provide protective immunity. If individuals wait until the peak of flu season, they risk contracting the virus before their immune system is fully prepared, potentially leading to severe illness, especially with the projected higher strain virulence.
Early vaccination also contributes significantly to community immunity, often referred to as herd immunity. When a large percentage of the population is vaccinated, it becomes more difficult for the virus to spread from person to person, protecting those who cannot be vaccinated, such as infants too young for the vaccine or individuals with certain medical conditions. This collective shield is particularly crucial when facing more virulent strains, as it reduces the overall viral load in the community and lowers the risk for everyone.
optimal timing for flu shots
While early is generally best, there is an optimal window for vaccination. The CDC typically recommends getting vaccinated by the end of October. However, with the 2025 flu season projections indicating higher virulence, getting vaccinated as soon as the vaccine becomes available, usually in late summer or early fall, is highly advisable. This ensures that peak immunity aligns with the anticipated onset and peak of flu activity. Delaying vaccination can leave individuals unprotected during the crucial initial phase of the season.
- August/September: Ideal time for most adults to get vaccinated.
- October: Still a good time, but earlier is preferred given projections.
- Children under 8: May require two doses given four weeks apart; early start is essential.
- Pregnant individuals: Vaccination at any stage of pregnancy protects both mother and baby.
The protective effect of the flu vaccine can wane over time, but for most individuals, early fall vaccination provides sufficient protection throughout the entire flu season. The benefits of early vaccination far outweigh any concerns about waning immunity, especially when faced with a potentially severe season. It is a proactive step that offers personal protection and contributes to broader public health safety.
In essence, early vaccination is paramount for personal protection and community resilience, particularly against the backdrop of the CDC’s alarming 2025 flu season projections. It enables timely immune response and strengthens herd immunity.
what to expect from the 2025 flu vaccine
The 2025 flu vaccine, like its predecessors, is meticulously developed to target the strains most likely to circulate during the upcoming season. Given the CDC’s projections of higher strain virulence, vaccine manufacturers and public health experts have worked diligently to ensure the vaccine offers the broadest possible protection. The vaccine formulation is based on extensive global surveillance data and predictive modeling, selecting strains that closely match those anticipated to be dominant. While no vaccine is 100% effective, the flu shot remains the most effective tool to prevent influenza and its severe complications. It is designed to reduce the risk of infection, and if infection does occur, to lessen the severity of symptoms and decrease the likelihood of hospitalization and death.
For the 2025 season, the vaccine will likely be quadrivalent, meaning it protects against four different flu viruses: two influenza A viruses and two influenza B viruses. This comprehensive coverage is crucial in a season where multiple virulent strains are expected to be active. The vaccine is safe and effective for most individuals aged six months and older, including pregnant women and those with chronic health conditions. Minor side effects, such as soreness, redness, or swelling at the injection site, low-grade fever, or aches, are common and typically resolve within a day or two. These are signs that the immune system is building protection.
types of flu vaccines available
Several types of flu vaccines are typically available, catering to different age groups and health needs. Understanding the options can help individuals make informed decisions in consultation with their healthcare providers.
- Standard dose inactivated flu shot: Administered via injection, suitable for most individuals.
- High-dose flu shot: Specifically designed for people aged 65 and older, offering a stronger immune response.
- Adjuvanted flu shot: Also for those 65 and older, containing an additive to boost immune response.
- Recombinant flu vaccine: Egg-free option, suitable for individuals with egg allergies.
The development process for each year’s flu vaccine is a global collaborative effort involving scientists, public health agencies, and manufacturers. This rigorous process ensures that the vaccine is as effective and safe as possible, providing a vital layer of defense against influenza. With the 2025 projections, the emphasis on receiving the most appropriate vaccine for one’s age and health status is more pronounced than ever.
In conclusion, the 2025 flu vaccine is formulated to combat anticipated virulent strains, offering robust protection against infection and severe outcomes. It is a safe and highly recommended preventative measure.
public health recommendations and guidelines
In light of the 2025 flu season projections, the CDC and other public health authorities are reinforcing a comprehensive set of recommendations and guidelines to minimize the impact of the anticipated higher strain virulence. Beyond early vaccination, these guidelines emphasize a layered approach to protection, recognizing that no single measure is foolproof. Individuals are encouraged to adopt a suite of preventative behaviors that collectively reduce the risk of transmission and illness. These recommendations are designed to be practical and easily integrated into daily routines, fostering a culture of health and preparedness within communities.
The guidelines also stress the importance of staying informed and responsive to local health advisories, as flu activity can vary by region. Public health campaigns will continue to educate the public on symptom recognition, when to seek medical care, and appropriate actions to take if symptoms develop. This includes strategies for managing illness at home to prevent overwhelming healthcare facilities, while also ensuring that those who need critical care receive it promptly. The overarching goal is to empower individuals with the knowledge and tools to protect themselves and their loved ones throughout the flu season.
key public health strategies
- Vaccination: Primary and most effective preventive measure.
- Hand hygiene: Frequent washing with soap and water or using alcohol-based hand sanitizer.
- Respiratory etiquette: Covering coughs and sneezes with a tissue or elbow.
- Staying home when sick: Preventing further spread of the virus.
- Cleaning and disinfecting: Regularly sanitizing frequently touched surfaces.
These strategies are not new, but their importance is amplified when facing a flu season with potentially more virulent strains. Adherence to these guidelines is a collective responsibility that contributes to the health and safety of the entire community. Public health officials will be working closely with schools, businesses, and healthcare providers to disseminate these recommendations and support their implementation.
To conclude, public health recommendations for the 2025 flu season extend beyond vaccination, advocating for a holistic approach to prevent transmission and mitigate the impact of virulent strains through informed individual and community actions.
preparing your family and community
Preparing for a flu season with higher strain virulence involves a multifaceted approach that extends beyond individual vaccination to encompass family and community-level readiness. For families, this means not only ensuring everyone eligible receives their flu shot early but also developing a household illness plan. This plan might include identifying a dedicated sick room, stocking up on necessary medications and supplies, and making arrangements for childcare or elder care should a caregiver become ill. Discussing the importance of hand hygiene and respiratory etiquette with children can instill good habits that protect the entire family. Open communication with schools and workplaces about their flu season policies can also help in planning and preparedness.
At the community level, preparedness involves supporting public health initiatives, participating in local vaccination drives, and promoting accurate health information. Community leaders, schools, and businesses play a vital role in disseminating CDC guidelines and encouraging adherence. Establishing clear communication channels for health advisories and resource availability can help manage potential outbreaks effectively. The collective action of a well-informed and prepared community can significantly reduce the overall burden of a severe flu season, protecting its most vulnerable members and maintaining essential services.
creating a family flu plan
- Get vaccinated: Ensure all eligible family members receive the flu shot.
- Stock up: Have fever reducers, pain relievers, tissues, and fluids on hand.
- Identify a sick room: Designate a space to isolate ill family members.
- Discuss hygiene: Reinforce handwashing and cough/sneeze etiquette.
- Plan for care: Arrange for backup childcare or elder care if primary caregivers get sick.
Engaging in these preparatory steps not only provides a sense of control but also builds resilience against potential health challenges. A prepared family is a protected family, and a prepared community is a healthier community. The effort invested in preparation now can yield significant benefits in terms of reduced illness, fewer complications, and a more stable environment during the flu season.
In summary, preparing your family and community for the 2025 flu season requires comprehensive planning, including early vaccination, household illness strategies, and active participation in public health efforts to foster collective resilience against virulent strains.
staying informed and proactive
In an environment where influenza strains are predicted to be more virulent, staying informed and proactive is paramount for protecting individual and public health. The flu landscape is constantly evolving, and official sources like the CDC are the most reliable channels for up-to-date information. Regularly checking the CDC’s website, local health department advisories, and trusted news outlets can provide timely updates on flu activity, vaccine availability, and any new recommendations. Being proactive means not only acting on these advisories by getting vaccinated early but also adopting a continuous mindset of vigilance regarding personal health practices and environmental hygiene.
Proactive engagement also involves advocating for health within your social circles, encouraging friends, family, and colleagues to take preventive measures. Sharing accurate information and dispelling misinformation can contribute significantly to community-wide protection. Furthermore, understanding the signs and symptoms of influenza and knowing when to seek medical attention is crucial. Early diagnosis and treatment, particularly for high-risk individuals, can prevent severe outcomes. This includes being aware of antiviral medications that can be prescribed by a doctor to treat flu illness, especially if started early in the course of the infection.
resources for reliable flu information
- Centers for Disease Control and Prevention (CDC): Official source for flu data and recommendations.
- Local health departments: Provide region-specific flu activity updates and resources.
- World Health Organization (WHO): Offers global flu surveillance and pandemic preparedness information.
- Healthcare providers: Your doctor or local clinic can offer personalized advice and vaccination services.
Maintaining a proactive stance means being prepared to adapt to changing circumstances throughout the flu season. This adaptability, combined with consistent adherence to public health guidelines, forms the strongest defense against a potentially challenging flu season. The collective effort of an informed and proactive populace is the most effective way to mitigate the impact of higher strain virulence and ensure community well-being.
Ultimately, remaining informed through reliable sources and taking proactive steps, such as early vaccination and adherence to health guidelines, is vital for navigating the 2025 flu season’s projected higher virulence effectively.
| Key Point | Brief Description |
|---|---|
| Higher Virulence Predicted | CDC projects 2025 flu strains will cause more severe illness and complications. |
| Early Vaccination Urged | Get vaccinated as soon as vaccine is available for optimal protection and herd immunity. |
| Comprehensive Protection | 2025 vaccine targets four strains, reducing infection risk and severity. |
| Family & Community Readiness | Develop household plans and support public health initiatives. |
frequently asked questions about the 2025 flu season
Higher strain virulence indicates that the circulating influenza viruses in 2025 are predicted to cause more severe illness. This can lead to increased symptoms, a higher likelihood of hospitalizations, and a greater risk of complications such as pneumonia, impacting both individual health and healthcare systems.
Early vaccination is crucial because it allows your immune system enough time (about two weeks) to develop protective antibodies before the flu season peaks. With projections of more virulent strains, being protected early can significantly reduce your risk of severe illness and contribute to community immunity.
The 2025 flu vaccine is expected to be quadrivalent, protecting against four different flu viruses. It is designed to reduce the risk of infection, lessen symptom severity if you do get sick, and decrease the chances of hospitalization and death, even against more virulent strains.
Everyone aged six months and older should get vaccinated. There are various types, including standard, high-dose, and adjuvanted options for seniors, and egg-free recombinant vaccines. Consult your healthcare provider to determine the most appropriate vaccine for your age and health status.
In addition to early vaccination, practice good hand hygiene, cover coughs and sneezes, stay home when sick, and regularly clean frequently touched surfaces. These measures collectively help prevent the spread of the flu and protect your community, especially against virulent strains.
conclusion
The CDC’s health advisory regarding the 2025 flu season projections serves as a vital alert for communities across the United States. With the anticipation of higher strain virulence, the emphasis on early vaccination is more critical than ever. This proactive measure not only safeguards individual health by minimizing severe illness and complications but also bolsters community immunity, protecting vulnerable populations. Adhering to public health guidelines, preparing families, and staying informed through reliable sources are equally important steps in mitigating the impact of a potentially challenging flu season. By taking collective action and prioritizing preventive care, we can all contribute to a healthier and more resilient environment in the face of evolving influenza threats.





